Diabetes is the leading cause of new cases of BLINDNESS among working-age Americans. Diabetes affects nearly 10% of American adults. EyeHealth Northwest physicians and surgeons are trained to diagnose and care for patients with Diabetes. Routine medical vision exams are recommended to maintain and prevent vision loss. The prevalence of diabetes in the United States has been estimated to be at least 9.6% of adults. Obesity, which is a major contributing factor, has risen 57% since 1991.
Diabetic Retinopathy
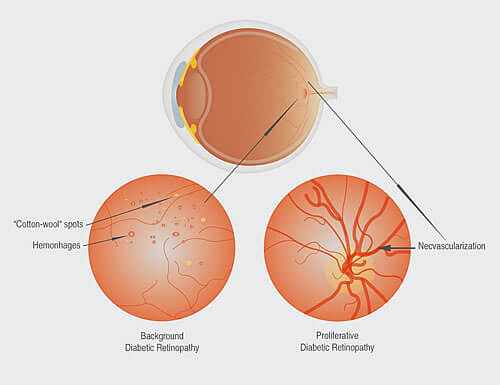
Diabetic retinopathy is a complication of diabetes that is caused by abnormal changes in the retina. The retina is a nerve layer at the back of the eye that senses light and helps to send images to your brain. In diabetes, the blood vessels in the retina may leak fluid or blood, grow fragile brush-like branches and scar tissue. This can blur or distort the images that the retina sends to the brain. If you have diabetic retinopathy, at first you may not notice changes to your vision. But over time, diabetic retinopathy can get worse and cause vision loss. Diabetic retinopathy usually affects both eyes.
Managing Diabetic Retinopathy
Today, with improved methods of diagnosis and treatment, only a small percentage of people who develop diabetic retinopathy have serious vision problems. With careful monitoring, your ophthalmologist can begin treatment before sight is affected. Laser and operative surgery are highly effective treatments for diabetic retinopathy, but your attitude and attention to medications and diet are also essential in dealing with the disease. The risk of diabetic retinopathy is related to many factors particularly the duration of diabetes and level of diabetes control. Other factors may aggravate the risk and severity of diabetic retinopathy. Control of these medical issues is the first-line treatment to prevent diabetic retinopathy. Medical issues and risk factors include:
- uncontrolled blood pressure
- elevated cholesterol and triglycerides
- kidney disease
- anemia
- smoking
- pregnancy

