The following information is intended to supplement your medical visit with your ophthalmologist. This document will help you understand cataracts, the risks of cataract surgery, and the type of replacement lens options. If you have additional questions after reading this, please be sure to ask your surgeon.
What is a cataract?
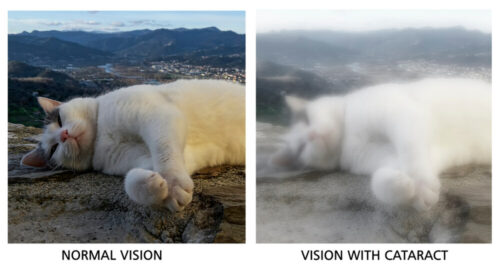
The eye is similar to a camera in that an image is “focused” on the back of the eye by the cornea, the lens, and sometimes with the aid of your glasses. When the normally clear lens becomes cloudy it is called a cataract. This can cause the image that falls on the back of your eye to be blurry. Cataracts are very common and usually become worse with time.
What symptoms do cataract cause?
Cataracts cause decreased vision and often cause symptoms of glare. Cataracts can make it difficult to see well enough to drive or read. Sometimes cataracts can cause double vision. Cataracts can also cause colors to appear dull or washed out. A new pair of glasses will not usually improve these symptoms.
What causes a cataract?
Most cataracts are simply caused by aging, although many people develop cataracts as early as their late 40s or 50s. About 50% of Americans aged 65-74 and 70% of those aged 75 or over have some degree of cataract.
Other causes of cataracts include:
• Genetics
• Diabetes
• Trauma
• Inflammation
• Sunlight or radiation exposure
• Exposure to medications such as steroids
• Smoking
How are cataracts treated?
The definitive treatment is surgery. During surgery, a small incision is made in the eye. The lens is broken into multiple pieces with an ultrasound machine and removed. This technique is called phacoemulsification. As part of the same procedure, a new clear artificial lens (intraocular lens or IOL) is used to replace the old lens and provide focusing power to the eye. This new lens improves vision because it is clear and not cloudy like the cataract.
How do you decide if it is time for Cataract surgery?
Your ophthalmologist will examine you and discuss how significant the cataract appears. Your ophthalmologist will also examine the rest of your eye to make sure there are no other reasons for your visual complaints. If the cataract is significantly affecting your ability to drive safely, read, or live comfortably because of your vision, it may be a good time to consider surgery. The decision to pursue surgery is based on your individual needs; your ophthalmologist can help you decide if the benefits of surgery appear to outweigh the risks of surgery. If you have other disorders of the eye impacting your vision, such as age-related macular degeneration, cataract surgery may improve your vision, but any pre-existing disease may limit your final visual outcome.
What can you expect before surgery?
Your surgeon will need to have some measurements of the eye prior to your surgery. These measurements are critical to help determine what power of lens to insert into the eye during surgery.
Contact lenses can mold the shape of your cornea and can make the above measurements less accurate. You must be out of your contact lenses for a period of time PRIOR to good measurements being taken. Your surgeon will advise you how long to stay out of your contact lenses, prior to taking measurements. This will depend on if you wear hard or soft contact lenses. If you have dry eyes, optimizing this prior to getting measurements including the use of artificial tears is recommended. Discuss this with your surgeon. Your doctor may prescribe medicated drops to begin using before your surgery.
What can you expect on the day of surgery?
Cataract surgery is performed on an outpatient basis in state-of-the-art eye surgery facilities. Your doctor and surgical team will make every effort to help you feel comfortable before, during, and right after your surgery. The procedure itself takes less than half an hour; however, the whole process takes 2-3 hours. Light sedatives are given to provide a relaxing experience and you remain awake during the procedure. The eye is “numbed” with an anesthetic solution. If you are nervous (this is normal!), an intravenous sedative can be given to you, which will help you to feel more relaxed. Depending on the regulations of the facility you are having surgery, you will be asked to not have any liquids or food for a defined period prior to your surgery. These rules allow sedatives to be given more safely.
What can you expect after the surgery?
You are expected to have minimal to no pain following the surgery. Your vision may be blurry after the surgery and you may be light-sensitive. It is common for you to feel a foreign body sensation for days. Your pupil may be dilated for 1-2 days afterward. It is common to see some shimmering in the periphery of your vision after surgery; this usually gets better with some time.
Your doctor will prescribe eye drops that are often used for a month after your surgery. These drops will help the eye be more comfortable, heal properly, and reduce the risk of infection. You will be given an eye shield to wear over the eye for the first 24 hours after surgery. The shield will also be needed when sleeping for the week following your surgery.
For the first week after surgery, avoid eye rubbing and heavy lifting. This avoids unnecessary pressure on the eye. Take things easy for 1-2 weeks after the surgery. Do not go swimming or use a hot tub for 2 weeks after the surgery. Most people take a week off from work after the surgery (this may not be necessary depending on your job specifics).
If you have a cataract in the other eye and it is bothersome, you can proceed with the second eye surgery once the first eye is healed, if this was your plan with your doctor. You are not obligated to do the surgery on the second eye.
Your prescription for glasses will be prescribed approximately 3-4 weeks after your eye surgery. Check with our expert optical staff at our optical shops for a convenient selection of non-prescription glasses that can be helpful until a prescription pair is given to you.
How do I know which Intraocular Lens (IOL) to choose?
There are multiple types of lenses that can be used during surgery. Below is a brief description of the options. Choosing the right lens can be complex; the choice of what lens is best for you should be made after a thorough understanding of your options and a careful discussion with your ophthalmologist. Here are the main options to choose from:
A. Standard IOL (with three options, see below)
B. Astigmatism correcting IOL
C. Multifocal
D. Extended Depth of Focus
E. Accommodating
A. Standard IOL
A standard IOL also referred to as “monofocal” or “single focus,” gives very good clarity of vision and is the most common IOL chosen. Insurance companies often cover the cost of a standard IOL. With a monofocal lens patients often choose one of three options:
Option 1: Correcting for distance vision in both eyes
Option 2: Correcting for near vision in both eyes
Option 3: Monovision (one eye distance, one eye near)
Read more about these three options:
Monofocal option 1: Correcting for distance vision in both eyes
Most patients who have a standard IOL choose to have the lens correct their distance vision as best as possible. A small glasses correction for distance may still be needed, especially if you have astigmatism (see below). In this option, you will still need glasses for near (e.g. reading) and intermediate (e.g. computer) work.
Monofocal option 2: Correcting for near vision in both eyes
Some patients who have a standard IOL choose to have the lens corrected for their near vision as best as possible. In this situation a patient may not need to wear glasses for near (unless they have astigmatism); however, they will likely need glasses to drive (or other tasks to see at distance or even intermediate distance); glasses will be needed for optimum clarity.
Monofocal option 3: Monovision (one eye distance, one eye near) Monovision is when one eye is corrected for distance vision and the other eye is corrected for near vision in an attempt to decrease your dependence on wearing glasses. It is often recommended to first try monovision with contact lenses to see if you can adapt to this type of vision. Some find it too difficult to adjust to each eye working differently, while many enjoy the benefits of this option.
B. Astigmatism Correcting IOL
Astigmatism simply means that the front part of your eye, the cornea, is not perfectly spherical. It is very common, and for most people is not a sign of anything serious. Contact lenses or glasses usually correct astigmatism. A “toric” or “astigmatism correcting” IOL is an option for patients with moderate amounts of astigmatism. Choosing this option, if you have astigmatism, can reduce your need for glasses after your surgery. If you choose a standard lens implant (i.e. no astigmatism correction) and you have astigmatism, you could wear glasses to correct astigmatism.
However, if it is desirable to have better vision when you are NOT wearing glasses, you may want to consider a toric lens implant. Your surgery scheduler can provide you with a guide to the costs.
A different option (not related to IOLs) for correcting astigmatism involves creating Limbal Relaxing Incisions (or LRIs). Your surgeon may perform this at the time of cataract surgery. These are extra incisions in the cornea to help reshape the cornea and can reduce the amount of astigmatism. LRIs are also not covered by insurance.
C. Multifocal IOL
These lens options can help reduce your dependence on glasses. A multifocal lens offers multiple focus points, distance, intermediate, and near vision (different models have different near points). It is also available as a toric lens that can also correct astigmatism. There are many pros and cons for the options in this category and these lens choices should be considered only if the eye has no other health problems.
Adjusting to this type of lens can take time (sometimes months). Other side effects could include glare (star-bursting) and halos as well as decreased contrast and color vision. Unfortunately, there are no guarantees that choosing a multifocal lens will eliminate your need for glasses. Some degree of glasses will often still be needed because there is no perfect lens technology available.
D. Extended Depth of Focus IOL
The extended depth of focus in this lens can provide a continuous range of high-quality vision from distance to intermediate and can allow patients to be more independent of glasses after cataract surgery, though some patients may still need glasses for near vision. It is also available as a toric lens that can also correct astigmatism. Some star bursting of lights has been reported with the use of this lens, though for most patients this is not severe. This lens may not be appropriate for everyone and it is important to have a thorough exam and discussion with your doctor about pre-existing conditions that may limit the use of this lens implant.
E. Accommodating IOL
The Crystalens is an artificial lens implant designed to treat presbyopia (the loss of intermediate and near vision) by modeling it after the natural lens in the human eye. This lens is designed to flex and accommodate in order to improve visual focus across all distances. Crystalens can reduce a person’s need for prescription glasses and reading glasses after cataract surgery. Many patients have greater freedom from glasses after surgery, compared to a standard or monofocal IOL. Patients still may require glasses after receiving this lens.
Trulign Toric is an artificial lens implant designed to treat presbyopia and correct astigmatism when implanted during cataract surgery. It is similar in design to the Crystalens, but has been modified to include correction for astigmatism. This allows more precise correction of distance vision for patients with astigmatism and also improves the vision for intermediate and near tasks. With Trulign Toric, many patients experience a broader range of vision and enjoy increased independence from glasses, compared to a standard or monofocal IOL.
from glasses, compared to a standard or monofocal IOL.
Will I still need glasses after surgery?
Most patients will still need to wear glasses for optimal vision after cataract surgery. However, your doctor can often reduce your glasses prescription (i.e. the thickness of your glasses can significantly be improved) and potentially decrease your dependence on glasses after surgery.
If you have a cataract, your cataract prevents you from seeing well even with glasses. The goal of cataract surgery is to improve your vision, although glasses are often still needed for optimized vision in different visual situations. As discussed above, there are multiple options that can help reduce your dependence on glasses. However, there is no guarantee that cataract surgery can completely eliminate your need for glasses, regardless of lens choice, even though some lenses reduce your likelihood of dependence more so than others.
After your cataract surgery, if you desire greater independence from your glasses, you may consider laser refractive surgery (e.g. LASIK) to improve your uncorrected vision. This is a “cosmetic” type of procedure; therefore the cost will not be covered by your insurance and will be an “out of pocket” expense. The great majority of patients do not need this option.
Does insurance cover Cataract Surgery?
Most medical insurances cover cataract surgery costs per plan specifications when it is considered medically necessary. If you are in a managed care plan, your insurance plan may need to authorize the surgery.
If you have Medicare coverage, please note that they cover some of the costs of surgery and a portion of a pair of glasses following the surgery, but they do not cover the refraction (test measuring your vision correction).
Any fees not covered by insurance (co-pay, deductible, co-insurance, or other uncovered amounts) are due at the time of service. EyeHealth Northwest accepts cash, checks, Visa, MasterCard, Discover, American Express, and Care Credit. Your surgery scheduler will discuss the cost estimate for your particular case.
What are the risks of Cataract Surgery?
There is no such thing as risk-free surgery; although, in general, cataract surgery is considered very safe. When the potential benefits of surgery outweigh the potential risks, your surgeon can help you decide if the procedure is for you. In general, 95% of patients will notice an improvement in vision after cataract surgery. The risks of a serious complication after surgery are generally low: approximately 1-2%. The risk of a sight-threatening infection after surgery is approximately 1/3,000. The risks of blindness from surgery vary highly and can be between 1/1,000 and 1/1,000,000. There may be some conditions in your eye that could create greater risks, and your surgeon will discuss them as they pertain to you.
Some of the risks in the following list are very rare but added for the purpose of inclusivity. If you want to know more information, please talk to your surgeon. Risks from cataract surgery can include, but are not limited to: bleeding, infection, glaucoma, droopy eyelid, retinal detachment, corneal swelling, retina swelling, cosmetically unacceptable outcome, pain, adverse reaction to sedative or anesthetics, abnormal light reflections, light sensitivity, decreased vision, permanent loss of all vision, worsening of dry eye, need for contact lenses, double vision, worsening of floaters and need for more surgery. Your surgeon will provide you with a consent form to read prior to the surgery, and the risks will be further detailed in that document. Please ask if you have further questions.
Once removed, can a Cataract come back?
No. Your cataract will never grow back. However, in many patients, a film can grow behind the lens which can cloud the vision months or years after the surgery. A laser can be used to improve the vision in this situation. Ask your ophthalmologist about details.
What is the lens implant made of?
Acrylic is the most common lens material, but sometimes silicone or other advanced lens materials. Each lens has specific indications and the doctor determines which lens is best suited for you based on a number of factors.
How long will the lens implant last?
The intraocular lens is placed permanently in your eye and will not wear out. Rarely, if the lens implant moves out of position or is the wrong power, it is removed or replaced.
Can my eye reject the lens implant?
No. Since the IOL is not living tissue, the body cannot reject it.
Who should I call if I have a problem after surgery?
If you have pain, especially a dull ache, this is a worrisome sign. Please call us right away. Other symptoms we would want to know about are decreasing vision, flashing lights, or a shade in vision. Even if it is after hours or during the weekend please call us at the designated number provided. It is always better to call us if you are worried. It is very important to all of us at EyeHealth Northwest that you are well taken care of and safe.

